J Biomed 2016; 1:26-31. doi:10.7150/jbm.16953 This volume Cite
Research Paper
Tailored Brushing Method (TBM): An Innovative Simple Protocol to Improve the Oral Care
1. Department of Oral and Maxillofacial Sciences, “Sapienza” University of Rome, Italy;
2. Tecnologica Research Institute, Crotone, Italy.
* These Authors equally contributed to this article.
Received 2016-7-23; Accepted 2016-9-1; Published 2016-9-20
Abstract
Background. The objective of this study is to describe and assess the effectiveness and acceptability of a modern tailored protocol of oral hygiene, based on the concordance between professionals and patients, and based on the proper choice of best tools for oral hygiene regardless of the technique used. This new method has been called Tailored Brushing Method (TBM).
Material and methods. Two groups of adult patients (n=200) were involved in this research, according to specific inclusion criteria. Test group followed the indications of the new Tailored Brushing Method, while control group was involved in a standard protocol of oral hygiene with the suggestions of a brushing technique and the typical approach based on the compliance. Plaque Index, bleeding on Probing index and patients' acceptability of the methods (Visual Analog Scale) were assessed at different time points. Descriptive and statistical analyses were performed.
Results and conclusions. Test group had statistically lower Plaque Index and Bleeding on Probing after 30 days, in comparison with control group. Test group expressed a better acceptance of the new tailored method. This research suggests to use a tailored approach to oral hygiene, overcoming the need of patient's compliance, often affected by bias such as alteration of the protocols and wrong brushing maneuvers.
Keywords: Oral hygiene, tooth-brushing, dental home care, tailored approach.
Introduction
A proper protocol to prevent the bacterial biofilm formation is strategic for oral health. It's well described in the literature that mechanical removal of dental plaque is the primary action able to prevent aggressive forms of gingivitis and periodontitis. 1
Current manual brushing techniques, such as the “Bass modified” one, are based on old concepts of oral hygiene and, however, they are commonly focused on specific movements and stereotyped timings finalized to disrupt the oral biofilm on teeth surface, independently from the instruments you are using and from the technique you are following.
Nowadays, we have many companies producing modern tools for oral hygiene, such as toothbrushes with easy grip handles, flexible stem, different head sizes, rounded bristles with a hardness range from medium to extra soft. Dental research has improved the effectiveness of modern toothbrushes, taking into consideration anatomy and physiology of teeth and periodontal tissues. However, such improvements have been not followed by new revised protocols.
Scientific evidence suggests that tooth brushing alone is less effective if compared to brushing with additional cleaning of interproximal areas; moreover, interproximal brushes are more effective than other interproximal cleaning tools (wire, stick floss, etc.). 1-3
Colorimetric assays using plaque disclosing agents, such as erythrosine, have been progressively integrated into the common protocols aimed to verify the correct use of brushing techniques.4 Although this assay and similar methods have been typically aimed to help patients to see and disrupt dental plaque, however, up to date the effectiveness of the mainly used maneuver of oral hygiene are still depending from the ability of patient to use such instruments correctly. This means that it's relatively important the technique you use and the level of patient's compliance if the ability of patients is variable and decreases over time.
In this paper we will introduce a new approach to oral care: a patient-specific oral hygiene protocol here named "Tailored Brushing Method" (TBM). TBM advises that dental hygienists and patients should share the protocol to be used, choosing together the most suitable tools to reach every dental surface: this joint therapeutic approach will lead to a better tooth brushing.5 According to scientific literature, TBM strongly suggests the use of interproximal brushes combined to toothbrush; moreover, TBM strongly suggests to professionals that they carefully should analyze gingival biotype, dental morphology, dental occlusion, patient's manual skill and personality profile.
The main objective of this study is to describe and assess the effectiveness of the firstly described tailored protocol entirely based on the concordance between professionals and patients, and based on the proper choice of best tools for oral hygiene regardless of the technique used. This new method has been called Tailored Brushing Method (TBM). TBM has been compared with the standardized oral brushing guided by disclosure tablets and requiring the patient's compliance.
Material and methods
This is a randomized, controlled pilot study. The main aim was to observe the differences between 2 groups of patients randomly involved in this study: Plaque Index 6 (PlI) and Bleeding on Probing (BoP) scores were used to assess the clinical difference between groups. Patient's satisfaction was investigated also, by using a VAS scale.
Selection of study population
Inclusion criteria
Selected patients were aged from 25 to 65 years old. All signed an informed consent describing the treatment to perform. Each patient had at least 20 teeth, and have been selected patients affected by mild to moderate gingivitis.7
Exclusion criteria
The following categories of patients were excluded from this study: smokers, pregnants, patients with mental disorders, patients under anti-tumoral therapy, patients under anticoagulant therapy, patients under biphosphonates therapy, patients affected by immunological disorders, with severe diabetes, patients showing dental erosion and/or abrasion and patients with fixed or mobile orthodontic appliances or prostheses.
Sample size
The study was carried out in the university hospital of Rome “Sapienza” and the recruited patients are representative of the macro area of central Italy.
We set an Alpha First Type Error of 0.05 and a test power of 90. We also hypothesized a number of patients who could not collaborate equal to the 10% of patients.
We recruited 200 patients so to allocate 100 of them in the Test group (G1) and 100 in the Control group (G2).
Randomization
The enrolled subjects were assigned to the two arms of the trial through a computerized program of randomization.
Clinical protocol
Ethics of experimentation
The procedures in the study related to conducting, execution and documenting follow the ethical principles listed in the Declaration of Helsinki and its subsequent revisions. The study was conducted according to the Italian and EU laws. Furthermore, all eligible patients received complete informations about the study and signed an informed consent.
Clinical data collected
We investigated some parameters such as: Plaque Index (PlI) and Bleeding on Probing (BoP) scores, following WHO guidelines.
Visual Analog Scale was administered to evaluate the acceptability of the applied oral hygiene methods.
Test group was made from 100 patients asked to try our innovative Tailored Brushing Method (TBM).
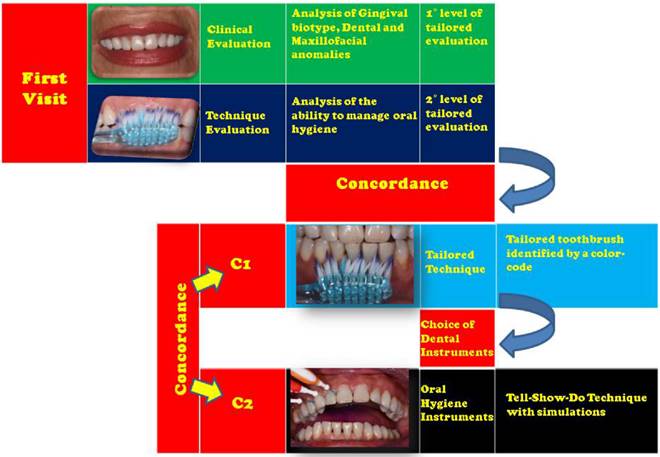
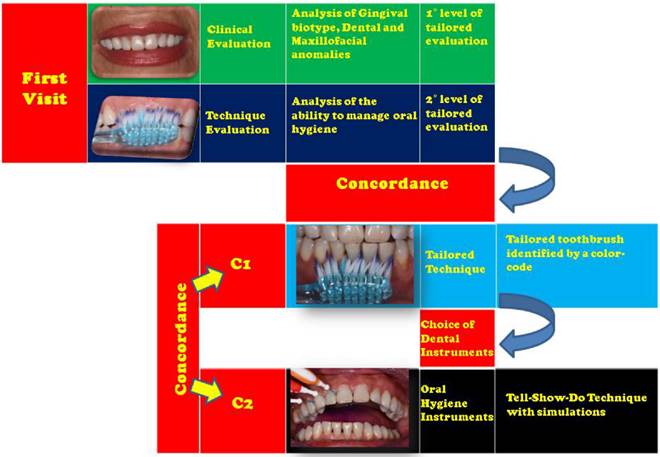
A synoptical figure describing about the T.B.M.- tailored brushing method.
Tailored Brushing Method (TBM)
The proposed Tailored Brushing Method (TBM) is based on a 2-stages decisional process (Fig. 1). First stage is the baseline: in this time, we evaluate the clinical characteristics of our patient, with a particular attention to the gingival biotype, to dental anatomy and to presence of diastemata; it's important to assess the whole oral condition by using clinical observation, plaque test, as well as new technologies useful to early detect developing pathologies affecting teeth surface. Moreover, in this stage we will ask patient to show us how he usually manage his oral hygiene: this is to understand the patient's habits, so to check which points are not brushed through his daily dental hygiene procedures and so to understand what instruments we need to use with him.
On the base of these evaluations, we need to share our clinical analysis with patient so to get a mutual concordance on the protocol to adopt. The concept of "compliance", in which the patient passively incorporates and learns some stereotyped movements, is here innovated with the concept of "concordance" which presupposes an active interaction between the patient and the healthcare provider.
Second stage is splitted in 2 concordances: C1 and C2
C1 is closely related to the techniques of oral hygiene to be used during professional treatments as well as during domiciliary oral care. C2 is instead related to the choice of toothbrush and interdental brush.
TBM requires that dental hygienists and patients choose the most suitable tools to reach every dental surface, including interproximal spaces or areas commonly inaccessible with traditional techniques, and that they jointly agree to perform a proper brushing, by means of a toothbrush with an arrangement bristle in tufts disposed on multilevel, with angled orientation, and a narrower conformation of the working part.5
In agreement to the scientific evidence, TBM requires that interproximal brushes are ever used in association with the toothbrush; of course, the choice of tools is patient-tailored. Tools are important to be accurately chosen: The arrangement of the bristles is preferable that it is on different levels and with different conformations: an effective conformation has bristles arranged in a "V" shape, in fact, such a morphology is able to reach the tooth surface and the gingival sulcus even in patients with orthodontic appliance.
With regard to disposable interdental brushes, flexible rubber ones are very useful, for the greater practicality of use and for the lower exposure to risk of papillary trauma in those cases with very tight interproximal spaces.
The handle of tools must be non-slip and the neck should have a good degree of flexibility.
In this pilot study, we selected patients with no limitation of manual ability, we therefore focused our attention on manual toothbrushes, selected in the light of the authors' experience and previous trials about the biomechanical analysis of bristles and toothbrushes.
The study
Test group (G1) patients were provided with the following instructions for home maintenance: biofilm disrupting twice a day for two minutes with technologically advanced toothbrush and interdental brush: an ergonomic handled interproximal brush will fill the patient's technical weaknesses.
When we have to treat patients affected from gingivitis, we will choose a toothbrush with two different levels of bristles (Gum Technique Pro Compact Medium): a layer of very fine tapered bristles with the last bristled narrower than the others; this conformation is studied to help patients to clean the gingival sulcus. A central layer of bristles will be designed to clean the tooth surfaces.
Interproximal brushes (Gum Travler) size will be chosen after the proper assessment of patient's anatomy: different sizes will be easily identifiable by codified colors.
The instruments we will choose for each patient during the first visit will be showed and explained with a tell-show-do technique. Professionals need to clearly explain the importance of using the right tools for different clinical situations, showing the use of selected tools with the aid of a mirror and plaque disclosure tablets. Patients will be also asked to brush under the operator supervision. Patients were asked to perform home oral care with the same procedures as described.
Control group (G2) was only required to clean their teeth as commonly they use to do, with the aid of colorimetric technique (plaque disclosure tablets).
Patients in the trial were followed in two time points:
Time 0 (baseline)
Recruitment of patients was performed in accordance with inclusion and exclusion criteria at the First Observation Dental Unit of the of Oral and Maxillofacial Sciences Department of “Sapienza” Rome University.
Since our purpose was to investigate the efficacy of a new home maintenance protocol, at T0 BoP was collected for each patient using a periodontal probe PCP 15 UNC. All the enrolled patients were then treated by a trained operator with ultrasonic scaling with deplaquing using airpolishing with glycine powder and ultrasonic scaling with universal insert.
PlI with the aid of a bitonal plaque detector was collected for each patient after the professional oral hygiene intervention to confirm the optimal level of plaque removal. Indices scores were recorded in a specific clinical survey form.
After clinical assessment, G1 patients received the Tailored Brushing Method instructions and tools as described above.
G2 patients were instead asked to use the bi-tonal plaque disclosure and to remove the “colored” biofilm with their usual dental hygiene tools and techniques without providing any further details; the authors emphasize how G2 patients were never instructed about the use of any professional brushing technique, infact, they were leaved free to manage toothbrush as they preferred to do.
G2 patients were made of patients similar for age and sex with respect of group G1, given that the allocation into the two groups was performed after the preliminary randomization.
After a minimum period of 30 days and no more than 35, data concerning Plaque Index (PlI) and Bleeding on Probing (BoP) were newly collected following the previously described methods (T1). Visual Analog Scale was administered in order to evaluate the acceptability of the used methods by the patients. The values obtained were elaborated in the statistical analysis.
Statistical analysis
Using all the collected data, it was executed a preliminary descriptive analysis. Categorical variables were summarized using frequencies in absolute and percentage value, while for continuous variables were calculated the measures of central tendency (mean, median, mode), the frequency distributions and confidence intervals at 95%.
To assess the presence of association between categorical variables was conducted the statistical test Chi-square both in aggregate and on subgroups based on gender, age.
For continuous variables, they were performed parametric tests (Student's t) for comparison of averages. The variables regarding the response of treatment (PlI and BoP), expressed as variations between the times, were tested with Student's t test for paired data. The level of significance was set at 0.05.
Results
An overall number of 200 patients were enrolled in the study. At the end of follow-up there were no drop-outs. Therefore, the final sample was composed by 200 subjects, 100 in the test group G1 and 100 in the control group G2.
Plaque Index
At recall, Plaque Index level varied significantly in the two arms (P = significant). Assuming Plaque Index=0 at baseline in all patients due to the professional scaling and deplaquing, test group had at T1 statistically lower Plaque Index level than control group (15% vs. 34%). In Table 1 are reported PlI values.
Moreover, using bi-tonal plaque disclosure tablet to distinguish the recent deposits from older ones, patients in the control group mostly showed both old and newly formed biofilm. On the other hand, coloring of the plaque in test group patients showed an accumulation limited to the last 24 hours.
Variations and clinical significance in plaque index (PI) in both Groups.
| Test Group | Control Group | Significance | |
|---|---|---|---|
| T (0) | 0 | 0 | |
| T (1) | 15% | 34% | Yes |
Bleeding on Probing
The Bleeding on Probing index variation is extremely significant (P<0.001) in both arms, thus indicating the overall effectiveness of professional and home care oral hygiene. In Table 2 are reported BoP values in the two groups. Better effectiveness of the G1 Tailoring Protocol than the G2 standardized method is perceived in the statistically significantly higher reduction of BoP clinical scores from T0 to T1 in the test group patients compared to the control group. With regards to topographic distribution, BoP reduction is not significantly different in upper or lower arch in both experimental arms.
Acceptability
Visual Analogue Scale scores revealed that 90% of patients in the test group expressed good acceptance of the proposed Tailored Brushing Method, significantly better than the control group patients, who expressed acceptance in 60% of cases.
Discussion
In this research we compared two different techniques of oral hygiene. We selected colorimetric technique as a control since this is the most valued approach described in recent literature.1-6 This approach can be biased being too patient dependent, potentially leading to inadequate plaque removing.6 On the other hand, the proposed Tailored Brushing Method focuses specific patient characteristics thus aiming at a predictable result in term of oral hygiene.
It is striking that no studies are available in order to update oral hygiene techniques with the existing toothbrush technologies. This study has the plus of describing a procedure associated to modern instrumentation. However, this research has some weaknesses, such as the limited number of involved patients.6,7
Variations and statistical significance in bleeding on probing (BoP) in both Groups.
| Variable Bleeding-Upper Arch | |||
|---|---|---|---|
| GROUP | CHANGE IN MEDIA | STANDARD DEVIATION | |
| Test | -1.03 | 0.65 | P |
| Control | -0.30 | 12.30 | |
| Variable Bleeding-lower Arch | |||
| GROUP | CHANGE IN MEDIA | STANDARD DEVIATION | |
| Test | -0.87 | 0.50 | P |
| Control | -4.7 | 0.28 |
In our opinion several reasons could explain our results. First of all, the evaluation of psychological aspect of patient represents an important way to approach the oral hygiene education.1-4 It is clear that adherence to protocols is a crucial aspect to be considered in oral hygiene training. This approach allows the patient to be followed in all the dental hygiene steps. In addition, a dental hygienist evaluates dexterity of the patient so to indicate a suitable instrumentation. Finally, some clinical aspects, such as dental occlusion, dental alignment, gingival biotype, presence of diastema, presence of dental erosion or recession, and orthodontic or prosthodontic appliances, allow to elaborate a tailored approach for each patient.
In our study all patients maintained a satisfactory level of oral hygiene at home. This can be partially explained by the shortness of time elapsing from T0 (oral hygiene and education) to T1 (30 days). The greater reduction of Bleeding on Probing index in the test group patients compared to the control group is consistent with the Plaque Index scores, and show a high effectiveness of the proposed customized approach, that lead to a higher adherence, satisfaction and actual clinical improvement of oral hygiene variables.
Besides, the reported observed differences in the plaque disclosure pattern in the two experimental groups, suggest a different biofilm stage. In fact, patients in the control group showed an older biofilm than those in the test group. This indicates possible deficiencies and inaccuracies in traditional standard home techniques, outdone by the introduction, in the Tailored Brushing Method, of personalized brushing and interproximal hygiene, thus completing the accuracy in home oral hygiene.
Conclusions
In conclusion, this research indicates that a tailored approach can lead to a successful result in patients with regard to their level of adherence and efficacy to an oral hygiene customized method.
In Protocol TBM we integrated the potential of advanced technologies with the needs of clinical practice.
We believe that the professional should recognize and treat any abnormal condition oral hygiene individually: this means that the trader has to interact with the patient's needs to create empathy, but above all he must use the minimally invasive technology, and be familiar with these technologies all the scientific, ethical, social, and economic. Only under these conditions you can choose a type of personalized treatment and shared with the patient.
The challenge for the future is to build experiences on a large scale, increasing attention to the level of understanding of how the technologies are an integral part of the therapies. Communication becomes not only verbal and para-verbal, but also a summation of concordances and performances directed to the patient's well-being.
Further studies will be needed to confirm and strengthen our results, implementing the application of the Tailored Brushing Method to the different patient needs.
Competing Interests
The authors have declared that no competing interest exists.
References
1. Van der Weijden GA, Hioe KPK. A systematic review of the effectiveness of self-performed mechanical plaque removal in adults with gingivitis using a manual toothbrush. J Clin Periodontol. 2005;32:214-228
2. Drisko CL. Periodontal self-care: evidence-based support. Periodontology 2000. 2013;62:243-245
3. Slot DE, Dörfer CE, Van der Weijden GA. The efficacy of interdental brushes on plaque and parameters of periodontal inflammation: a systematic review. Int J Dent Hyg. 2008;6:253-264
4. Marrelli M, Amantea M, Tatullo M. A comparative, randomized, controlled study on clinical efficacy and dental staining reduction of a mouthwash containing Chlorhexidine 0.20% and Anti Discoloration System (ADS). Ann Stomatol. 2015;6:35-42
5. Slot DE, Wiggelinkhuizen L, Rosema NAM, Van der Weijden GA. The efficacy of manual toothbrushes following a brushing exercise: a systematic review. Int J Dent Hyg. 2012;10:187-197
6. Loe H. The gingival index, the plaque index and the retention index systems. J Periodontol. 1967;38:610-616
7. Morris AJ, Steele J, White DA. The oral cleanliness and periodontal health of UK adults in 1998. British Dental Journal. 2001;191:186-192
Author contact
![]() Corresponding author: Silvia Sabatini, RHD. Via delle Azalee 18 00172 Rome (Italy). Telephone +393495061580 - Fax +390649976638 Email: silvia.sabatini2it.
Corresponding author: Silvia Sabatini, RHD. Via delle Azalee 18 00172 Rome (Italy). Telephone +393495061580 - Fax +390649976638 Email: silvia.sabatini2it.